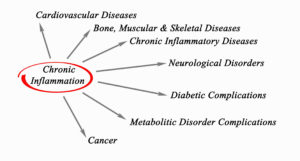
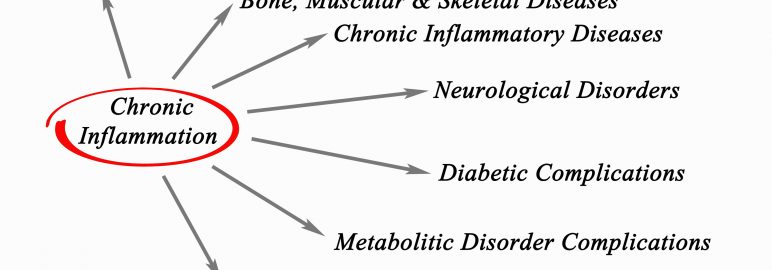
In Part 1 of this series I provided an overview of inflammation in the body. In this part, I’ll cover the research on various diseases apparently related to inflammation. In Part III, I’ll talk about the key to successful aging and what you can do to fight chronic inflammation.
In Part 1 of this article I talked about the relationship between a “highly processed, high-fat, high-sugar meal” and inflammation in our bodies. I also mentioned how the medical community is beginning to focus more on the role of such inflammation in different diseases.
I mentioned that in an article in the July 2017 issue of Mayo Clinic Health Letter, Brent Bauer, M.D., noted several diseases in which inflammation may or does play a part, including: rheumatoid arthritis, lupus, polymyalgia rheumatica, asthma, cancer, and inflammatory bowel diseases.
While treatment options tend to vary for these conditions, none has a cure. However, research indicates there is one thing we can all do to decrease our chances of getting these diseases or improving our symptoms: eat fewer animal products (or avoid them altogether).
For example, researchers found that “a high-fat diet may contribute to chronic inflammatory diseases of the airway and lung.”
So to help improve airway disorders, such as asthma, it may help to eat a low fat diet. How low? Well, a high-fat diet in that study was defined as 1 g fat/1 kg body weight, which would mean about 62 grams of fat for a person who weighs around 140 pounds. Most Americans consume that amount and more every day on a standard diet.1
Diet also plays a role in conditions such as arthritis, which actually refers to joint pain or joint disease, comprising more than 100 different types of conditions. (I covered arthritis in the May issue of the newsletter. Check it out here.)
The following information is specific to rheumatoid (inflammatory) arthritis.
A 2002 study in the Journal of Alternative and Complementary Medicine, showed that “patients with moderate-to-severe rheumatoid arthritis, who switch to a very low-fat, vegan diet can experience significant reductions in RA symptoms.”2 A 1999 study published in the American Journal of Clinical Nutrition showed that “some patients with rheumatoid arthritis can benefit from a fasting period followed by a vegetarian diet.”3
The inflammatory reactions of arthritis appear to trigger when susceptible people put animal proteins in their body. Their immune systems react by producing antibodies to the animal product but attack their own bodies instead. For example, when you eat animal cartilage your body instead attacks your own cartilage. That’s called meat-induced joint attack.
Another possibility is the immune complexes formed by the meat proteins and our antibodies may migrate into our joints and trigger inflammation. Whatever the action, somehow meat is playing a role.4
Several compounds from meat, including fat, were also associated with an increased risk of Crohn’s disease and ulcerative colitis, as shown through a systematic scientific review of the role of diet in inflammatory bowel disease. At the same time, high fiber, fruit and vegetable intakes were associated with decreased risks of one or both these diseases.5
Crohn’s disease is an inflammatory bowel disease in which your body attacks your own intestines. It affects more than a million Americans. There is no cure. Research focuses on controlling symptoms.
A 2013 article in Cell Immunology noted that there is no definitive medical or surgical therapy for inflammatory bowel diseases like Crohn’s. However, research has demonstrated that a more plant-based diet has offered the best results to date for relapse prevention. The results were better than those obtained by drugs, including pricey biological agents.6
The summary from Part 1 of this article and the research noted here is that a diet low in processed food can decrease inflammation in your body and lower your risk of inflammatory-based diseases. At the same time, a diet high in whole plant foods such as fruits, vegetables and whole grains, can improve symptoms if you already have one or more of the diseases and decrease your risk even further if you don’t.
While the link between diet and inflammation is becoming clearer, there is still much to be learned. Meanwhile, the evidence seems to support consumption of whole grains, vegetables, fruits and legumes for better health. So, the next time you’re out, grab a salad, add some legumes and whole grains, and hold the high-fat dressing.
References
- Rosenkranz SK, Townsend DK, Steffens SE, Harms CA. Effects of a high-fat meal on pulmonary function in healthy subjects. Eur J Appl Physiol. 2010 Jun; 109(3):499-506.
- J. McDougall, B. Bruce, G. Spiller, J. Westerdahl, and M. McDougall. Effects of a very low-fat, vegan diet in subjects with rheumatoid arthritis. J Altern Complement Med, 8(1):71-75, 2002.
- Am J Clin Nutr. 1999 Sep;70(3 Suppl):594S-600S. Rheumatoid arthritis treated with vegetarian diets. Kjeldsen-Kragh J.
- NutritionFacts.org. Accessed September 22, 2017.
- J K Hou, B Abraham, H El-Serag. Dietary intake and risk of developing inflammatory bowel disease: a systematic review of the literature. Am J Gastroenterol. 2011 Apr;106(4):563-73.
- S Bandzar, S Gupta, M O Platt. Crohn’s disease: a review of treatment options and current research. Cell Immunol. 2013 Nov-Dec;286(1-2):45-52.
Sorry, comments are closed for this post.